What is Caesarean Section ?
Caesarean section (C-section) is the delivery of a baby through a cut in the mother's lower abdomen and the uterus. Caesarean births are more common than most surgeries (such as gallbladder removal, hysterectomy or tonsillectomy) because a caesarean section may be life saving for the baby, or mother (or both). Caesarean birth is also much safer today than it was a few decades ago. Hence 'caesarean'; is not something that should scare you, as the ultimate goal is a healthy mother and healthy baby, regardless of the method of delivery. It is important to know a few things about caesarean section in order to be prepared for a caesarean birth if it does happen to you. The following section will help you to understand caesarean births better.
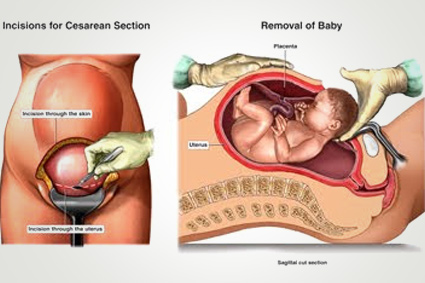
Caesarean section may be an emergency procedure or an elective and hence planned procedure. Peparation for the surgery may be done in the labour room or in the theatre itself. This includes putting a catheter into your bladder to drain urine, and an intravenous line (needle) into a vein in your hand or arm to give your body fluids and medications as required. You may be given an antacid orally, or injections like Perinorm or Ranitidine to reduce the level of acid in your stomach and prevent vomiting. Your abdomen and pubic hair will be shaved, and the area washed with an antibacterial solution. Suitable anaesthesia is given to you so that you are pain-free during the procedure. The doctor makes the skin incision first. This is either a vertical incision in the middle from below the navel up to the pubic bone. A transverse or bikinicut incision (called pfannesteil incision) from side to side just above your pubic hairline.
- After going through the various layers of the abdominal wall, and opening the bladder fold of peritoneum, the lower segment of the uterus is exposed.
- The incision is now made on the uterine wall, usually horizontal (side to side) this is preferred as it heals better and bleeds less. However, due to certain circumstances it may be necessary for your doctor to make a vertical incision on the uterus.
- The amniotic sac (bag of water) is broken and your baby is delivered either by hand or using forceps. At this point if you are under regional anaesthesia, you may feel some tugging, pulling or some pressure on the upper abdomen.
- The umbilical cord is clamped and cut, and your baby is handed to the neonatologist or nurse for evaluation.
- The placenta is detatched from the uterine wall and removed.
- The uterine incision is closed using sutures (usually) or staples, and bleeding is controlled.
- The abdomen is now closed, and the skin sutured. Depending on the initial skin incision, the skin may be closed with removable sutures, staples, or subcuticular (under the skin surface) dissolvable sutures.
- You may be given your baby to hold if you are feeling upto it, After observing your vital parameters (pulse, blood pressure, etc.) for some time you may be shifted to your room.
- The complete procedure takes about 45 minutes to one hour in an uncomplicated case. From the initial incision to delivery of the baby takes about 5 minutes, and the remaining time is taken for repairing your uterus and abdominal wall.
Anaesthesia and Pain Relief
Different measures may be used for pain relief before, during and after your caesarean.
Before Operation: If you had been in labour, you may have been taking medications for pain relief. If an epidural is already in place, for example when you have been in labour for a while before you needed a caesarean section, it is usually continued for the surgery.
During the surgery: Regional anaesthesia, that is one, which acts to block the pain only at the operative area (and below), is usually preferred. This may be an epidural, typically being continued from labour analgesia.
Another type of regional anaesthesia is spinal anaesthesia, which can be given more quickly, provides better pain relief and is usually preferred if an anaesthetic is not already given. The advantages of regional anaesthesia include the fact that you are not unconscious only the lower half of your body is numb. Hence, you are aware of when your baby is delivered and may even see / hold the baby before he / she is shifted out of the operating room. More than that, some risks of general anaesthesia like aspiration, respiratory complications and delayed breastfeeding are also avoided. It may be possible that a regional anaesthetic cannot be given to you for medical reasons. Another possibility is that, in an emergency caesarean. There may not be enough time to give a regional block. In such cases general anaesthesia is given, where you will be completely unconscious during the surgery. Some women, who are apprehensive about the surgery may infact opt for general anaesthesia as a personal choice. Your doctor, in conjunction with the anaesthesiologist (doctor giving the pain relief) will be the right person to help you decide what is best for you.
Why are Caesareans Done ?
Before you can understand the various causes for which caesarean section may be required, you should know that basically there are two broad categories of operation:
Emergency Caesarean Section: Where you may have been in labour for a while before the decision is taken, or some problem develops that makes urgent delivery necessary in the interest of your baby, or your health.
Common indications for emergency caesarean sections are
- Foetal distress.
- Dystocia or non-progress of labour.
- Bleeding from your placenta.
An emergency surgery is always more risky than a planned procedure. This may be because you are not on empty stomach, or there are life threatening problems like severe bleeding or rise in your blood pressure, or complete facilities like experienced anaesthetist / neonatologist / operative team / blood may not be immediately available.
This is one reason why your doctor may suggest a planned or elective caesarean section to you. If there are certain pre-existing conditions, which make it nearly certain that you will not be able to deliver safely vaginally, it may be better to do a planned procedure. This could be for reasons like
- Previous two or more caesareans.
- Placenta praevia.
- Mal-presentations of your baby etc.
Why Caesareans Births Occur ?
Let us now understand some of the reasons for which caesarean births may occur.
Dystocia: (difficult or abnormal labour patterns).
The causes of dystocia are many, but basically the end result is that labour fails to progress, is prolonged excessively, or gets arrested.
Your doctor may try measures like augmenting contractions with oxytocin, or rupturing the amniotic sac to improve the labour pattern. If these fail, however Caesarean section may be the only option.
Foetal distress: Your baby may not be tolerating the forces of labour well, and may show problems like irregularity or slowing of the heart rate, or acid in the blood. Sometimes greenish discolouration of the amniotic fluid (passage of meconium or foetal stools in utero) may be a sign of distress. If vaginal delivery cannot be completed quickly, a caesarean may be the best way to save your baby.
Mal-presentations: Unfavorable positions of the foetus in utero can make vaginal delivery difficult, dangerous or impossible.
These include:
- Transverse lie
- Shoulder presentation
- Oblique lie
- Breech presentation (buttocks first)
- Posterior face presentation
- Face presentation
- Brow presentation
Some of these conditions may be corrected before the onset of pains by a procedure called ‘external cephalic version’, by which your doctor attempts to turn the baby to the correct position. This may not be feasible or safe in all cases. Though, for breech, particularly if you have had a normal delivery earlier, it may be possible in some cases to deliver the baby vaginally. However, even without difficulties in delivery, breech babies have a less favorable outcome. Hence many doctors opt for planned caesarean. This is a problem, which needs prior discussion with your doctor.
Placental or cord problem : The placenta is the main connection between the mother and the foetus providing nutrition, oxygen and other essentials to the baby via the umbilical cord. Bleeding occurring from the placenta before delivery can be risky. It may be due to an abnormal location of the placenta ‘placenta praevia'. It may be due to early separation of a normally located placenta called ‘abruption placenta. These can endanger your life or your baby’s health. Hence a Caesarean section may be done. The umbilical cord may prolapse (come out) into the vagina before the baby’s birth. This is more common with malpresentations. Pressure on the prolapsed cord can lead to baby’s death. Hence an emergency caesarean section is usually required.
Cephalo-pelvic Disproportion or mismatch between the size of the baby and the birth passage. This may be due to abnormalities in the bony pelvis such as:
* A small or contracted pelvis r esulting from previous pelvic injury or fracture.
* A large sized baby where the baby is too big to deliver through the pelvis.
Remember, however, that these are relative terms and can be sometimes overdiagnosed. Proper evaluation of foetal and pelvic relative sizes is best done after 38 weeks or ideally at the onset of labour. Even if mild disproportion is suspected, your doctor may suggest a ‘trial of labour’ where a wait and watch policy is followed to see what the forces of labour can achieve. This may avoid unnecessary caesareans.
Other problems in the birth canal such as:
- A stenosed cervix.
- A thickly cervix which does not open up.
- Previous pelvic repair of a urinary or rectal fistula.
- Active herpes lesions of the genital tract.
These may be the reasons for your doctor suggesting caesarean section.
Maternal medical conditions may also call for a C-section. The conditions include:
- Pre-eclampsia or Pregnancy Induced Hypertension (PIH) is a leading cause of maternal and foetal problem, even today. Due to uncontrolled blood pressure or impending complication likes eclampsia, HELP syndrome
it may be necessary to opt for caesarean birth. - Maternal diabetes in pregnancy is also associated with problems, which may make caesarean birth a safer option.
- Other medical illness like severe asthma, certain types of cardiac diseases, etc. may also preclude labour as mother, baby or both may not be able to tolerate labour well.
Previous Caesarean Delivery
This is now becoming a very common indication for repeat caesarean section. Most patients with one prior caesarean delivery may deliver safely vaginally in the later pregnancies. This is more likely if the prior caesarean section was for a non-recurrent or temporary condition of that pregnancy, such as:
- Malpresentation
- Foetal distress
- Bleeding from the placenta
The options should be discussed by you and your doctor prior to onset of labour. If a vaginal birth trial is opted for certain guidelines need to be followed discussed later in this section.
In some cases, you and your doctor may opt for an elective or planned repeat caesarean. This is more commonly done if you have had:
- More than one caesarean previously
- Your baby is now larger
- Not in a favorable presentation
The type of prior caesarean is also important, as with an incision, the risks of attempting VBAC are more.Other uterine surgeries done in the past such as myomectomy or septum resection may also influence the decision for type of delivery.
Risks Involved
Caesarean births are much safer now than they were a few decades ago, In fact, hardly a century ago, having a caesarean was like a death sentence for the mothers. Today, the procedure carries a ‘risk’ of less than 1 in 2500. Yet, this risk is 4 times more than the risk of death after a normal vaginal delivery.
However, when talking about risks, one must keep in mind that statistics show that most people die at home or in bed. That doesn’t mean that by not staying home or not sleeping you can escape the inevitable!
While talking of risks what needs to be seen in the risk-benefit ratio. The ultimate aim is to have a healthy mother and healthy baby. In a given situation, if the benefits offered by caesarean birth to the mother, the baby or both are more than the risks; the procedure needs to be done regardless. Individual medical conditions like uncontrolled blood pressure or profuse bleeding from the placenta may make a vaginal birth more dangerous for the mother.
Risk for the Mother
- Infection: Post-operative infection of the uterus, or nearby organs like the bladder may occur. Use of antibiotics has reduced this risk.
- Increased bleeding: Some blood loss is inevitable at birth, but it is twice as much at caesarean as compared to a vaginal delivery.
- Complications of the anaesthesia used
- Urinary tract: Difficulty in passing urine, urinary retention, infection may occur. Rarely, surgical damage to the bladder or ureters may occur, particularly in cases of repeated surgery.
- Bowel function: Post operatively, the bowel movements may become sluggish or slow down completely. This leads to distension, bloating and abdominal discomfort.
- Respiratory tract: Occasionally, due to aspiration of stomach contents, pneumonia may result. This is more common with general anaesthesia.
- Wound problems: There may be a blood clot or pocket of pus in one or more stitches. In more severe cases there may be infection of the whole abdominal wound, and partial or complete dehiscence (splitting open) of the wound.
- Blood clots: They may form in the leg veins, or collect in the uterus. Clots in the pelvis organs or veins may travel to the lungs causing embolism, a serious complication. This is reduced by early ambulation.
- Delayed recovery: The hospital stay after a caesarean birth is usually twice as long as after a vaginal birth. In case of a ‘bikini’ incision, the average stay is 5 days, with a vertical midline incision, it may be 7 days or more. Full recovery of daily activities may take 4 weeks or more.
- Long term: Increased chance of repeat Caesarean section.
Risk for the Foetus
- Prematurity: The baby may have been delivered too early if there was miscalculation of the due date. Sometimes, despite knowing that the baby will be premature, an emergency caesarean may be needed, such as, for bleeding from the placenta, uncontrolled hypertension, etc, in the mother’s best interest.
- Low Apgar Score: The baby may have depressed activity at birth, as measured by the Apgar score.
- This could be due to the anaesthesia, other medications, or pre-existing factors. This need not indicate any long-term problem, however.
Breathing difficulty: Transient tachypnoea of the newborn (rapid or irregular breathing) is more common with caesarean birth. This is thought to be due to lack of the ‘squeezing out’ of lung fluid, which occurs in vaginal births. This usually settles in a few days. - Foetal injury: Although this is rare, the baby may be accidentally nicked while the surgeon is opening the uterus. With malpresentations, or deeply engaged head (as in caesareans after a long and difficult labour ) there may be some trouble delivering the baby, a minor foetal bruising or injury.